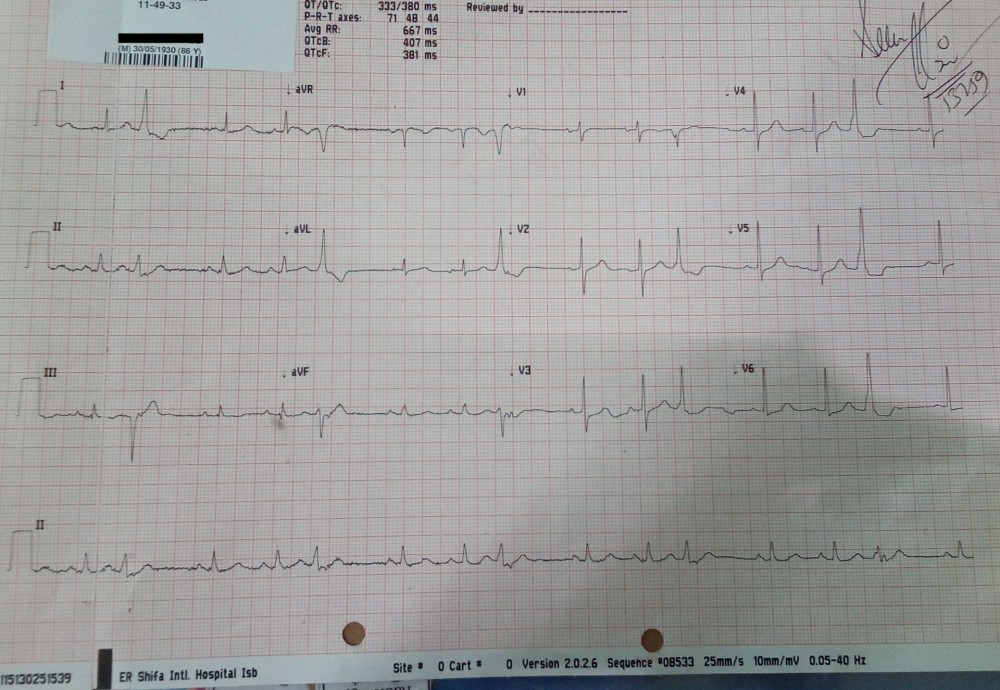
Regular or iregular?It can be seen that QRS complexes are clumped into groups, each comprising of three complexes. So its regularly irregular as marked in the following figure:
If irregular is it regularly irregular or irregularly irregular?

Main differential of such a rhythm would be sinus arrhythmia, Mobitz type II block, Atrial premature beats, Sinus arrhythmia is unlikely because, in sinus arrhythmia, the rate usually gradually slows and then gradually speeds up. There is no prolongation of PR interval as in mobitz type II block. Now have a look at p wave morphology of three beats in every group and the compensatory pause after it:

Are you thinking Atrial Trigeminy?
YES, you nailed it. If we notice the p wave morphology of every third beat its slightly different from the preceding p waves, and also its occurring earlier, compensatory pause after it and then restoration of sinus p wave in next cycle. So these are definitely Atrial Ectopics. Every third beat is atrial premature beat so pattern is Trigeminy.Atrial Ectopics:
These arise from ectopic pacemaking tissue within the atria. There is an abnormal P wave, usually followed by a normal QRS complex. PACs have the following features:- An abnormal (non-sinus) P wave is followed by a QRS complex.
- The P wave typically has a different morphology and axis to the sinus P waves.
- The abnormal P wave may be hidden in the preceding T wave, producing a “peaked” or “camel hump” appearance — if this is not appreciated the PAC may be mistaken for a PJC.
- PACS arising close to the AV node (“low atrial” ectopics) activate the atria retrogradely, producing an inverted P wave with a relatively short PR interval ≥ 120 ms (PR interval < 120 ms is classified as a PJC).
- PACs that reach the SA node may depolarise it, causing the SA node to “reset” — this results in a longer-than-normal interval before the next sinus beat arrives (“post-extrasystolic pause”). Unlike with PVCs, this pause is not equal to double the preceding RR interval (i.e. not a “full compensatory pause”).
- PACs arriving early in the cycle may be conducted aberrantly, usually with a RBBB morphology (as the right bundle branch has a longer refractory period than the left). They can be differentiated from PVCs by the presence of a preceding P wave.
- Similarly, PACs arriving very early in the cycle may not be conducted to the ventricles at all. In this case, you will see an abnormal P wave that is not followed by a QRS complex (“blocked PAC”). It is usually followed by a compensatory pause as the sinus node resets.
Classification:
PACs may be either:
- Unifocal – Arising from a single ectopic focus; each PAC is identical.
- Multifocal – Arising from two or more ectopic foci; multiple P-wave morphologies.
Patterns:
PACs often occur in repeating patterns:- Bigeminy — every other beat is a PAC.
- Trigeminy — every third beat is a PAC.
- Quadrigeminy — every fourth beat is a PAC.
- Couplet – two consecutive PACs.
- Triplet — three consecutive PACs.
Clinical Significance:
- PACs are a normal electrophysiological phenomenon not usually requiring investigation or treatment.
- Frequent PACs may cause palpitations and a sense of the heart “skipping a beat”.
- In patients with underlying predispositions (e.g. left atrial enlargement, ischaemic heart disease, WPW), a PAC may be the trigger for the onset of a re-entrant tachydysrhythmia — e.g. AF, flutter, AVNRT, AVRT.
Causes:
Frequent or symptomatic PACs may occur due to:- Anxiety.
- Sympathomimetics.
- Beta-agonists.
- Excess caffeine.
- Hypokalaemia.
- Hypomagnesaemia.
- Digoxin toxicity.
- Myocardial ischaemia
Comments
Post a Comment
Drop your thoughts here, we would love to hear from you