Thought 1: How to approach wide complex tachycardia?
Thought 2: What is the first line drug in this case?
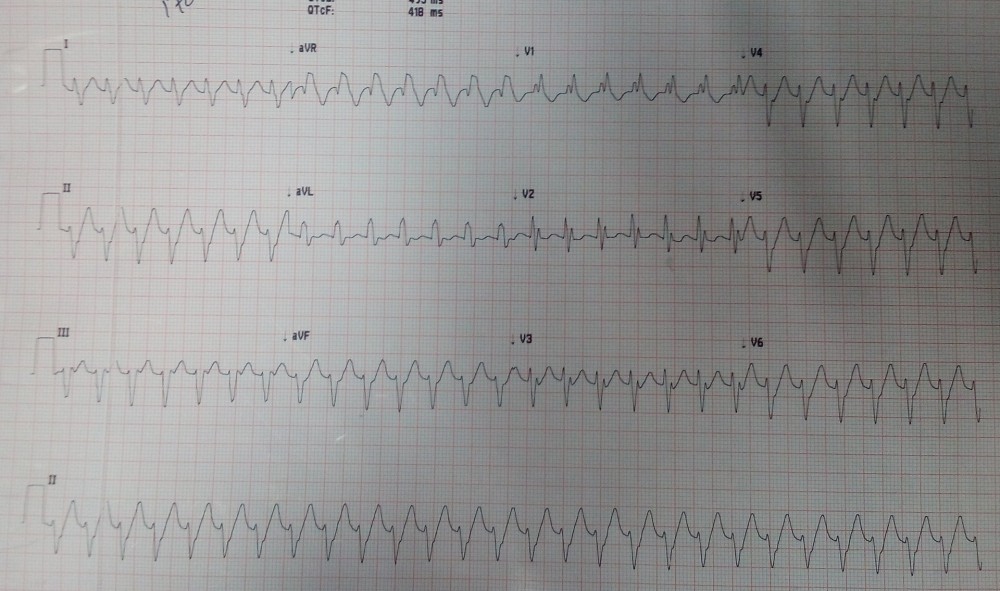
This ECG has wide-complex tachycardia(QRS duration=120msec) at a rate of 180 bpm with a RBBB pattern, left superior axis deviation and R-S interval is hardly 80msec suggesting Idiopathic Fasicular Left Ventricular Tachycardia (ILVT) and due to left superior axis deviation its Posterior Fasicular VT. Right ventricular outflow tract tachycardia is also differential here but it is usually with LBBB morphology. During wide complex tachycardia the differentiation between supraventricular and ventricular origin of the arrhythmia is important to guide therapy. Several algorithms have been developed to aid in this differentiation which we will discuss in next sections.
The patient was initially treated with successive rounds of synchronized DC Cardioversion, which were ineffective. Intravenous amiodarone, lidocaine and adenosine were also tried but did not terminate it. Finally, the patient received intravenous Verapamil, which terminated the tachycardia with resultant normal sinus rhythm. The patient was admitted and coronary angiography was done which showed clean coronaries. His hospitalization was uneventful and he was subsequently discharged home with the plan to return for a radiofrequency ablation.
Idiopathic Fasicular Left Ventricular Ventricular Tachycardia (ILVT):
Posterior fascicular VT by far accounts for the majority of ILVT, representing over 90% of cases. Often, ILVT is mistaken for supraventricular tachycardia with aberrancy. The surface electrocardiogram demonstrates tachycardia with a RBBB pattern and a left superior axis deviation. Other forms of ILVT include anterior fascicular VT presenting with a RBBB and right axis deviation as well as the more rare upper septal fascicular VT which can present with either a RBBB, left bundle branch block (LBBB), or a normal QRS.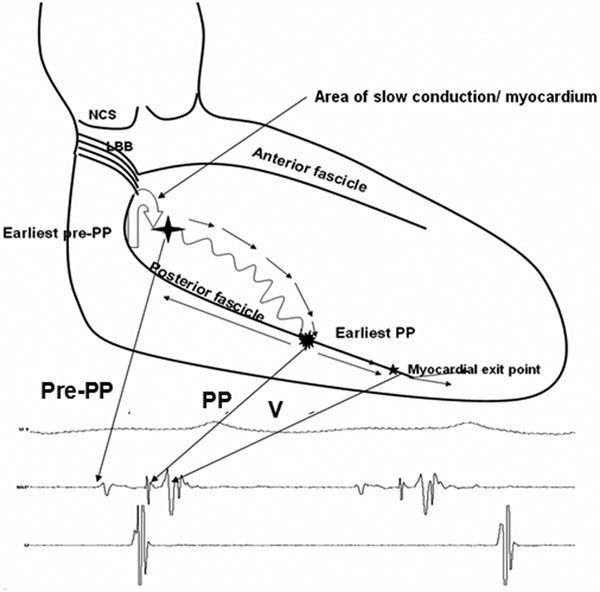
Above image showing Pre-Purkinje potential (pre-PP or P1) and Purkinje potential (PP or P2). The proposed antegrade circuit travels in the myocardial septum creating P1. The turnaround point occurs in the apical third of the left ventricle resulting in P2 as the impulse travels retrograde.
Anatomically, it is believed that the re-entrant loop for posterior fascicular VT involves a verapamil-sensitive septal myocardium that exhibits decremental properties from the base to the apex of the LV. It was demonstrated that there is a mid-diastolic pre-Purkinje potential (P1) and a pre-systolic potential (P2). P1 is described as a low frequency mid-diastolic potential during VT whereas P2 is described as a sharp, short-duration, high-frequency presystolic potential. The septal myocardium serves as the antegrade limb for the VT and is responsible for the creation of P1 during VT. The retrograde limb consists of either the posterior fascicle or its nearby tissue creating P2 during VT. It has traditionally been thought that P2 was created by a retrograde limb formed by the posterior fascicle. However, other studies have challenged this idea. Morishima have suggested that P2 may actually represent activation of the myocardial tissue in proximity to the fascicle. Kuo et demonstrated that ablation of ILVT did not result in fascicular block, leading the authors to conclude that the fascicle may not be involved in the re-entry circuit, simply the tissue adjacent to it. It has still not been completely elucidated whether the circuit is completely defined by fascicular tissue alone or whether there is a component of ventricular myocardium involved.
ECG Features of ILVT:
- Monomorphic ventricular tachycardia
- QRS duration 100 – 140 ms — this is narrower than other forms of VT.
- Short RS interval (onset of R to nadir of S wave) of 60-80 ms — the RS interval is usually > 100 ms in other types of VT.
- RBBB Pattern.
- Axis deviation depending on anatomical site of re-entry circuit
How to approach broad complex tachycardia:
Several ECG algorithms have been developed to differentiate wide QRS-complex tachycardias. Most of them performed very well in the population they were based upon. Brugada algorithm (below). This is the most commonly used algorithm. SN 89%, SP 59.2%.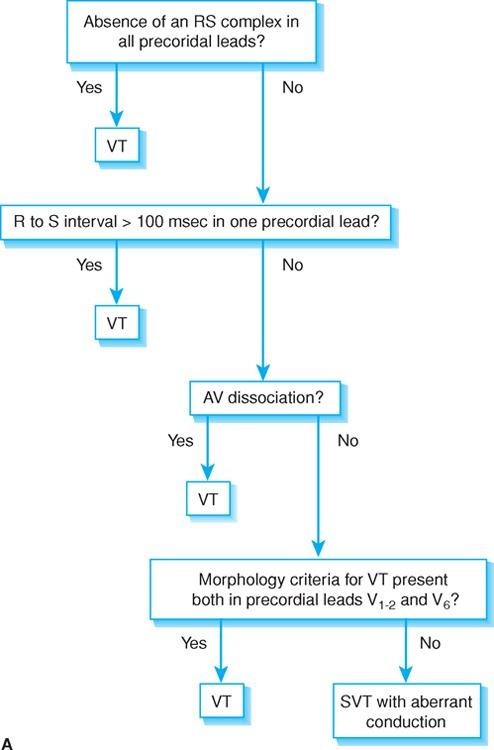
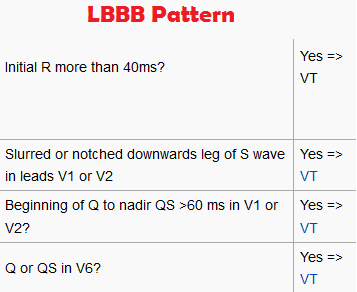
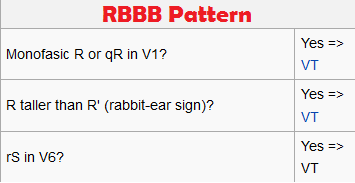
More advanced tips:
Ultra -Simple Brugada Criteria:
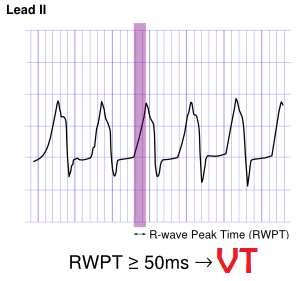
In 2010 Joseph Brugada et al. published a new criterion to differentiate VT from SVT in wide complex tachycardias: the R wave peak time in Lead II . They suggest measuring the duration of onset of the QRS to the first change in polarity (either nadir Q or peak R) in lead II. If the RWPT is ≥ 50ms the likelihood of a VT very high (positive likelihood ratio 34.8)
References:
- Lerman BB, Stein KM, Markowitz SM. Mechanisms of idiopathic left ventricular tachycardia. J Cardiovasc Electrophysiol 1997; 8:571–583
- Belhassen B, Rotmensch HH, Laniado S. Response of recurrent sustained ventricular tachycardia to verapamil. Br Heart J 1981; 46:679–682.
- Ramprakash B, Jaishankar S, Rao HB, Narasimhan C. Catheter ablation of fascicular ventricular tachycardia. Indian Pacing Electrophysiol J 2008; 8:193–202.
- Morishima I, Nogami A, Tsuboi H, Sone T. Negative participation of the left posterior fascicle in the reentry circuit of verapamil-sensitive idiopathic left ventricular tachycardia. J Cardiovasc Electrophysiol 2012; 23:556–559.
Comments
Post a Comment
Drop your thoughts here, we would love to hear from you