Aneurysm Versus Pseudo-aneurysm:
Introduction:
The terms like aneurysm and pseudoaneurysm often emerge, causing confusion and concern among patients and healthcare professionals alike. Understanding the disparities between these two conditions is crucial for accurate diagnosis, effective treatment, and improved patient outcomes.
Defining Aneurysm and Pseudo-aneurysm:
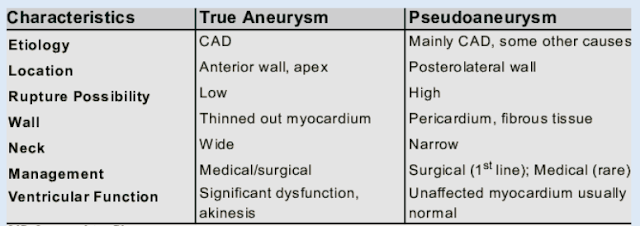
Aneurysm, a term derived from the Greek word for "dilation," refers to a localized, abnormal bulge or ballooning of a blood vessel wall. In the context of the heart, aneurysms typically occur in the arterial walls, such as the aorta or coronary arteries, due to weakened vessel walls or trauma.
On the other hand, pseudoaneurysm, also known as false aneurysm, represents a distinct entity. Unlike true aneurysms, which involve all three layers of the vessel wall, pseudoaneurysms result from a breach in the arterial wall with subsequent extravasation of blood into the surrounding tissue. This collection of blood forms a pulsatile hematoma that communicates with the arterial lumen through a small defect or tear.
Etiology and Risk Factors:
The development of aneurysms and pseudoaneurysms in the cardiac setting can stem from diverse etiologies and risk factors. Aneurysms may arise from atherosclerosis, genetic predisposition, inflammatory conditions like vasculitis, or infectious processes such as endocarditis. Trauma, including blunt or penetrating chest injuries, can also precipitate aneurysm formation.
In contrast, pseudoaneurysms often originate from iatrogenic causes, particularly invasive cardiac procedures such as coronary angiography, percutaneous coronary interventions (PCI), or cardiac surgery. Inadequate hemostasis at the arterial puncture site can lead to the formation of a pseudoaneurysm, emphasizing the importance of meticulous procedural technique and post-procedural monitoring.
Clinical Manifestations and Diagnostic Evaluation:
Both aneurysms and pseudoaneurysms can present with a spectrum of clinical manifestations, ranging from asymptomatic incidental findings to life-threatening complications. In the absence of symptoms, these cardiac abnormalities may be incidentally detected during imaging studies performed for unrelated reasons.
Symptomatic patients may experience chest pain, dyspnea, palpitations, or signs of cardiac failure, depending on the size, location, and complications associated with the aneurysm or pseudoaneurysm. Diagnostic evaluation typically involves a combination of non-invasive imaging modalities such as echocardiography, computed tomography (CT) angiography, magnetic resonance imaging (MRI), or invasive angiography for definitive characterization and localization of the pathology.
Management Strategies:
The management approach for aneurysms and pseudoaneurysms hinges on various factors, including the underlying etiology, anatomical considerations, clinical presentation, and patient-specific characteristics. In asymptomatic cases, a conservative monitoring strategy with regular surveillance imaging may suffice, particularly for small, stable lesions with a low risk of complications.
However, symptomatic or high-risk patients may necessitate active intervention to mitigate the potential sequelae associated with these cardiac abnormalities. Treatment modalities encompass pharmacotherapy for underlying conditions, endovascular techniques such as embolization or stent graft placement, or surgical repair, either through open-heart surgery or minimally invasive approaches.
Prognosis and Follow-up:
The prognosis of patients with cardiac aneurysms or pseudoaneurysms is contingent upon numerous variables, including the underlying pathology, the extent of cardiac involvement, the presence of comorbidities, and the timeliness and efficacy of therapeutic interventions. While some individuals may enjoy a favorable long-term outcome with appropriate management, others may encounter recurrent complications or progression of disease necessitating ongoing monitoring and tailored interventions.
Conclusion:
Distinguishing between aneurysms and pseudoaneurysms is pivotal for accurate diagnosis, optimal management, and improved patient outcomes. By elucidating the disparities in etiology, clinical manifestations, diagnostic evaluation, and therapeutic strategies associated with these conditions, healthcare providers can navigate the complex landscape of cardiovascular pathology with precision and proficiency, ultimately enhancing the quality of care delivered to individuals afflicted by these cardiac abnormalities.
#cardiology #radiology
Comments
Post a Comment
Drop your thoughts here, we would love to hear from you